Endometriosis is a chronic, often painful condition that affects millions of women worldwide. Among its various stages, Stage 4 endometriosis represents the most severe form, characterized by extensive tissue involvement and significant symptoms. Understanding Stage 4 endometriosis is critical for patients, caregivers, and healthcare professionals to ensure timely diagnosis, effective treatment, and improved quality of life.
In this comprehensive guide, we will explore what Stage 4 endometriosis is, its causes, symptoms, diagnosis, treatment options, complications, and ways to manage the condition effectively. We will also answer frequently asked questions to provide you with clear, evidence-based information.
What is Endometriosis?
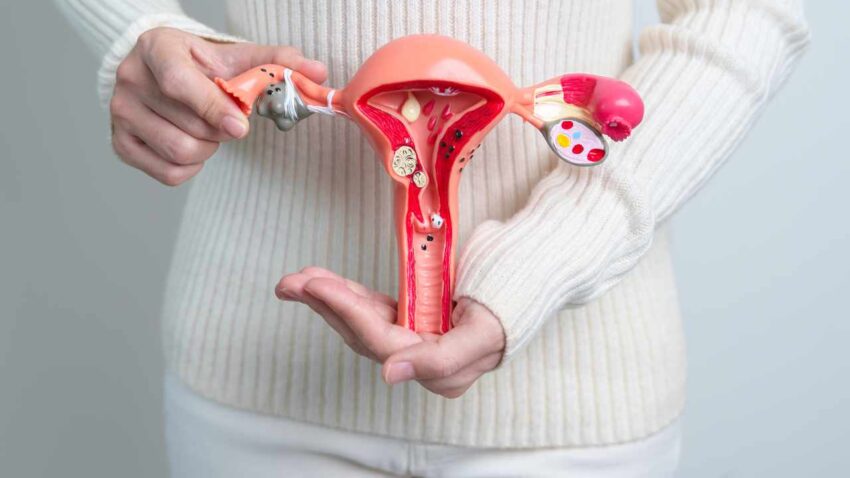
Before diving into Stage 4, it’s important to understand endometriosis itself. Endometriosis is a disorder where tissue similar to the lining inside the uterus (called endometrium) grows outside the uterus. This abnormal tissue growth can occur on the ovaries, fallopian tubes, pelvic lining, and other areas within the pelvic cavity. Rarely, it can be found beyond the pelvis.
This misplaced tissue continues to act as it normally would during the menstrual cycle — thickening, breaking down, and bleeding. However, because this tissue has no way to exit the body, it becomes trapped, causing inflammation, pain, scar tissue, and adhesions.
The Stages of Endometriosis
Endometriosis is classified into four stages by the American Society for Reproductive Medicine (ASRM):
-
Stage 1 (Minimal): Few small implants or lesions, little to no scar tissue.
-
Stage 2 (Mild): More lesions than Stage 1, deeper implants.
-
Stage 3 (Moderate): Many deep implants, small cysts on one or both ovaries, and presence of scar tissue.
-
Stage 4 (Severe): Extensive deep implants, large cysts on one or both ovaries (endometriomas), and significant scar tissue and adhesions.
The stage is determined during surgery, typically laparoscopy, and helps guide treatment and prognosis.
What Exactly is Stage 4 Endometriosis?
Stage 4 endometriosis is the most advanced stage of this condition. It involves:
-
Extensive lesions deeply infiltrating pelvic tissues.
-
Large endometriomas (also called “chocolate cysts”) on one or both ovaries. These cysts are filled with old, dark blood.
-
Dense adhesions and scar tissue that often cause organs in the pelvis to stick together, potentially distorting normal pelvic anatomy.
-
Possible involvement of bowel, bladder, and other pelvic structures.
Because of its severity, Stage 4 endometriosis is usually associated with severe pain, significant infertility issues, and other complications.
Causes and Risk Factors of Stage 4 Endometriosis
The exact cause of endometriosis, including Stage 4, remains unclear. However, several theories exist:
-
Retrograde menstruation: Menstrual blood containing endometrial cells flows backward through fallopian tubes into the pelvic cavity instead of leaving the body.
-
Coelomic metaplasia: Transformation of cells outside the uterus into endometrial-like cells.
-
Immune system dysfunction: Inability of the immune system to recognize and destroy misplaced endometrial tissue.
-
Genetic predisposition: Family history may increase risk.
-
Hormonal influences: Estrogen promotes the growth of endometrial tissue.
Risk factors that may increase the likelihood of developing advanced endometriosis include:
-
Early onset of menstruation (before age 11).
-
Short menstrual cycles (less than 27 days).
-
Heavy or prolonged periods.
-
Never giving birth.
-
Family history of endometriosis.
Symptoms of Stage 4 Endometriosis
Symptoms can vary widely, but Stage 4 endometriosis typically causes more severe and chronic symptoms, including:
-
Chronic pelvic pain: Persistent pain in the lower abdomen or pelvis, often worsening during menstruation.
-
Dysmenorrhea: Extremely painful periods.
-
Dyspareunia: Pain during or after sexual intercourse.
-
Infertility: Difficulty conceiving is common.
-
Painful bowel movements or urination: Especially during menstrual periods.
-
Fatigue: Due to chronic pain and inflammation.
-
Heavy menstrual bleeding or spotting between periods.
Due to the adhesions and organ involvement, some patients may experience bowel obstruction or urinary tract problems.
Diagnosing Stage 4 Endometriosis
Diagnosing Stage 4 endometriosis requires a combination of:
-
Medical history: Detailed discussion of symptoms.
-
Pelvic exam: May reveal tenderness, masses, or nodules.
-
Imaging studies: Ultrasound or MRI can identify endometriomas and some deep infiltrating lesions but are not definitive for all endometriosis lesions.
-
Laparoscopy: The gold standard for diagnosis. A minimally invasive surgery allows direct visualization of lesions and scar tissue. Biopsies can be taken for confirmation.
Treatment Options for Stage 4 Endometriosis
Treatment aims to relieve symptoms, improve fertility if desired, and prevent disease progression. Options include:
1. Medical Therapy
-
Hormonal treatments: These reduce or stop menstruation, which can decrease lesion activity and pain.
-
Birth control pills.
-
Gonadotropin-releasing hormone (GnRH) agonists and antagonists.
-
Progestins.
-
Danazol (less common due to side effects).
-
-
Pain medications: NSAIDs like ibuprofen help control pain.
2. Surgical Treatment
Because Stage 4 involves extensive adhesions and cysts, surgery is often necessary, especially for pain relief and fertility improvement.
-
Laparoscopic excision: Removal of endometriotic tissue and cysts while preserving organs.
-
Ovarian cystectomy: Removing endometriomas.
-
Adhesiolysis: Cutting adhesions to restore anatomy.
-
Hysterectomy and oophorectomy: Considered in severe cases or if childbearing is complete.
Experienced surgeons specializing in endometriosis are crucial for optimal outcomes.
3. Assisted Reproductive Technologies (ART)
For those struggling with infertility, in vitro fertilization (IVF) may be recommended.
Complications of Stage 4 Endometriosis
-
Infertility: Up to 50% of women with endometriosis face fertility challenges.
-
Chronic pain: Leading to impaired quality of life.
-
Bowel or bladder involvement: May cause obstruction or dysfunction.
-
Ovarian damage: Due to cysts or surgery.
-
Emotional and psychological impact: Anxiety, depression, and fatigue.
Managing Life with Stage 4 Endometriosis
Management is holistic and involves:
-
Pain management strategies.
-
Physical therapy.
-
Support groups and counseling.
-
Diet and lifestyle modifications to reduce inflammation.
-
Regular follow-up with healthcare providers.
References and Trusted External Links
Conclusion
Stage 4 endometriosis is the most severe form of this complex condition, characterized by extensive tissue involvement, large cysts, and significant adhesions. It often results in chronic pain and fertility issues, requiring a comprehensive, multidisciplinary approach for management. Early diagnosis and tailored treatment plans can significantly improve outcomes and quality of life for affected women.
If you suspect you have stage or have been diagnosed with Stage 4, consult with a gynecologist specialized in the for personalized care.
Frequently Asked Questions (FAQs)
Q1: Can Stage 4 endometriosis be cured?
Currently, there is no cure for endometriosis. However, treatments can manage symptoms and improve quality of life. Surgical removal of lesions can provide significant relief.
Q2: Is Stage 4 endometriosis life-threatening?
It is not life-threatening but can severely affect daily life due to pain and complications.
Q3: Can I get pregnant with Stage 4 endometriosis?
Fertility is often reduced, but many women with Stage 4 can conceive naturally or with the help of fertility treatments like IVF.
Q4: How is Stage 4 endometriosis different from earlier stages?
Stage 4 has more extensive disease, large cysts, and dense scar tissue, leading to more severe symptoms and complications.
Q5: What lifestyle changes can help manage symptoms?
Regular exercise, a healthy anti-inflammatory diet, stress management, and avoiding smoking can support symptom control.